How Venture Investment in Digital Health can
Reduce Bias and Break Poverty Cycles
Eddie Chan (MBA, Kellogg School of Management) *[email protected]u
Reduce Bias and Break Poverty Cycles
Eddie Chan (MBA, Kellogg School of Management) *[email protected]u
The wealth gap continues to widen in America. Those who lack the sufficient financial buffer often falter under the slightest economic strain, which has only been exacerbated due to COVID-19. This results in not only serving to keep those in the poverty cycle there, but also seeks to push those able to break out back into the loop. From a healthcare-specific perspective, the failure of the system to provide basic, affordable health solutions, regardless of income, continues to be a driving force in perpetuating inequality. Diseases such as kidney failure, cardiovascular disease, and mental illness continue to impact those in poverty at an increased rate, often due to lack of early detection. As AI diagnosis becomes more prevalent, we must ensure that data can be leveraged not only for economic policy purposes, but also for health diagnosis and treatments as well, in order to maximize the efficacy of resources deployed from impact investors. The interconnected nature of social, economic, and health issues represents an opportunity for the synergies in investments with focused impact lenses and greater effect towards overall social good.
What is the Poverty Cycle?
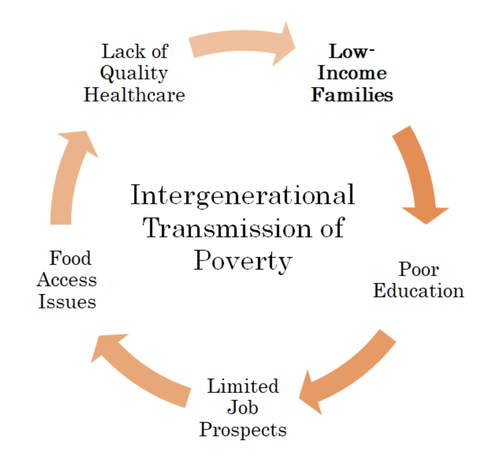
Based on 2018 census data (which inherently underestimates the results as it does not include the homeless population), the official US poverty rate is ~12%(1). Half of those, roughly 19 million people, were reportedly in deep poverty, which is defined as a household income below 50% of the poverty threshold ($24,600 for a family of four in 2017(2)). Social determinants of health have been the talk of the town as environmental, social, and governance (ESG) investing has gone mainstream. Those who can’t access quality education will end up with low incomes, leading to poor access to food and healthcare, further resulting in impoverished families; this carries on from generation to generation. Investing in functions (e.g. education, job placement, governmental programs) with direct ties to income generation has been shown to be successful at reducing poverty by nearly 50%(3) and is especially valuable for improving quality of life for children.
What is the Poverty Cycle?
Based on 2018 census data (which inherently underestimates the results as it does not include the homeless population), the official US poverty rate is ~12%(1). Half of those, roughly 19 million people, were reportedly in deep poverty, which is defined as a household income below 50% of the poverty threshold ($24,600 for a family of four in 2017(2)). Social determinants of health have been the talk of the town as environmental, social, and governance (ESG) investing has gone mainstream. Those who can’t access quality education will end up with low incomes, leading to poor access to food and healthcare, further resulting in impoverished families; this carries on from generation to generation. Investing in functions (e.g. education, job placement, governmental programs) with direct ties to income generation has been shown to be successful at reducing poverty by nearly 50%(3) and is especially valuable for improving quality of life for children.
However, despite gains in raising people’s income above poverty levels, it is quite easy for these individuals to fall back into this cyclical path. These snapshots obfuscate the real issue; instead of looking at end of year data points, we can see that a third of Americans were in poverty for at least two months in a 3 year period(4), highlighting the vulnerability of the larger lower-income population to financial hardships. Roughly half of those who get out of poverty will become poor again within five years(5). The fact that people continue to cycle in and out of poverty over the course of their lives underscores the need for support with all aspects of life that can plunge them back in.
So why is AI diagnostic care important?
It has been proven repeatedly that low incomes are strongly correlated (and even display causal relationships) with specific diseases. However, as discussed above, allocating resources purely to the income side of the equation overlooks the inverse issue- that health concerns can be the trigger point for individuals entering and reentering the poverty loop. In a longitudinal study on heart disease from 2007-2012, it was shown that 31% of the population that developed heart disease fell into income poverty vs. 15% from the group that did not develop the condition(6). This inverse relationship can be generally explained by the high cost of treatment and the time out of the workforce for these individuals. While social economic programs may serve to lessen the burden of those with job insecurity. It will be much more cost effective and drive better long-term outcomes if we can detect illnesses earlier and less expensively by using non-invasive methods, which, over time, would significantly slow or even prevent higher complexities of many illnesses that scale the costs, both financial and human, of our healthcare system.
Preventative/diagnostic health is and will continue to be a huge growth driver in the healthcare industry. As the industry shifts towards value-based care, an emphasis on diagnostics will have a positive influence on the quality of life of all patients. The early detection of various diseases allow for not only better treatment, but generally lower cost treatment over the lifetime of the patient. Data shows that the lifetime cost of a diabetic who receives regular diagnostic testing is $1,684 vs. $80,553 for a patient that is non-compliant(7). From a financial perspective, early diagnosis will alleviate the effects of the health-poverty trap.
With regards to low- to moderate-income (LMI) communities that face additional hurdles, alternative forms of non-invasive diagnostics can have an outsized impact. Lack of affordable care is the first obstacle to address; adults with family incomes less than $35k were 4x more likely to have no regular place to receive medical care vs. those with incomes greater than $100k (23% vs. 6%)(8). Secondly, distrust of the medical system frequently impacts healthcare consumption, even when it is made available; adults ages 50 to 75 with incomes below $15k were 2x more likely to have never been screened for colorectal cancer than those with incomes greater than $75k (43% vs 20%)(9). By leveraging data-based processes that allow the constant risk-assessment of entire populations, it is possible to introduce more pervasive disease monitoring. Trayt is a startup that monitors mental health through comorbidity assessments that provide a 360-degree view of patients. Early traction has shown improvements in compliance and reimbursement efficiency by 30%(10).
The aggregation of information will also incorporate social data and enable determinations without private health records, providing more targeted diagnostics that factor in the lifestyles of various communities. While this may drive results, usage of this type of information requires an emphatic approach to the skepticism towards monitoring and tracking felt by low-income populations. Access to and usage of private data, even without the input of private health records, warrants some level of privacy-related concern. MindRight is a startup focused on accessible and inclusive mental health support. Procedures and protocols for how coaches interact with students, what they communicate, when, and to what extent students are able to authorize coaches to report on specific information shared, gives the students/users a level of agency that garners trust long-term.
The potential value of impact venture capital
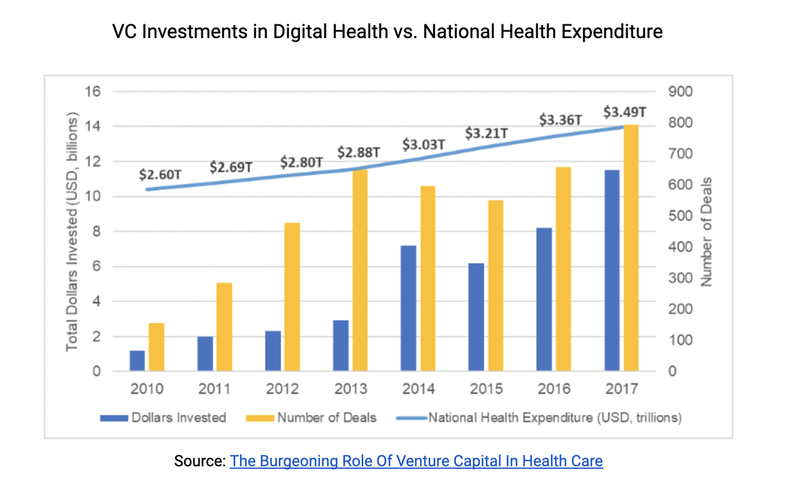
The scaling of preventative care makes it a great fit for venture capital, both from a consumer standpoint and a data collection business. The potential value of constant data collection through connected devices and backend algorithms and analytics to evaluate global health is enormous. This is borne out in the data- the dollars invested and number of deals VCs have made into digital health startups has been steadily increasing over the past decade.
So why is AI diagnostic care important?
It has been proven repeatedly that low incomes are strongly correlated (and even display causal relationships) with specific diseases. However, as discussed above, allocating resources purely to the income side of the equation overlooks the inverse issue- that health concerns can be the trigger point for individuals entering and reentering the poverty loop. In a longitudinal study on heart disease from 2007-2012, it was shown that 31% of the population that developed heart disease fell into income poverty vs. 15% from the group that did not develop the condition(6). This inverse relationship can be generally explained by the high cost of treatment and the time out of the workforce for these individuals. While social economic programs may serve to lessen the burden of those with job insecurity. It will be much more cost effective and drive better long-term outcomes if we can detect illnesses earlier and less expensively by using non-invasive methods, which, over time, would significantly slow or even prevent higher complexities of many illnesses that scale the costs, both financial and human, of our healthcare system.
Preventative/diagnostic health is and will continue to be a huge growth driver in the healthcare industry. As the industry shifts towards value-based care, an emphasis on diagnostics will have a positive influence on the quality of life of all patients. The early detection of various diseases allow for not only better treatment, but generally lower cost treatment over the lifetime of the patient. Data shows that the lifetime cost of a diabetic who receives regular diagnostic testing is $1,684 vs. $80,553 for a patient that is non-compliant(7). From a financial perspective, early diagnosis will alleviate the effects of the health-poverty trap.
With regards to low- to moderate-income (LMI) communities that face additional hurdles, alternative forms of non-invasive diagnostics can have an outsized impact. Lack of affordable care is the first obstacle to address; adults with family incomes less than $35k were 4x more likely to have no regular place to receive medical care vs. those with incomes greater than $100k (23% vs. 6%)(8). Secondly, distrust of the medical system frequently impacts healthcare consumption, even when it is made available; adults ages 50 to 75 with incomes below $15k were 2x more likely to have never been screened for colorectal cancer than those with incomes greater than $75k (43% vs 20%)(9). By leveraging data-based processes that allow the constant risk-assessment of entire populations, it is possible to introduce more pervasive disease monitoring. Trayt is a startup that monitors mental health through comorbidity assessments that provide a 360-degree view of patients. Early traction has shown improvements in compliance and reimbursement efficiency by 30%(10).
The aggregation of information will also incorporate social data and enable determinations without private health records, providing more targeted diagnostics that factor in the lifestyles of various communities. While this may drive results, usage of this type of information requires an emphatic approach to the skepticism towards monitoring and tracking felt by low-income populations. Access to and usage of private data, even without the input of private health records, warrants some level of privacy-related concern. MindRight is a startup focused on accessible and inclusive mental health support. Procedures and protocols for how coaches interact with students, what they communicate, when, and to what extent students are able to authorize coaches to report on specific information shared, gives the students/users a level of agency that garners trust long-term.
The potential value of impact venture capital
The scaling of preventative care makes it a great fit for venture capital, both from a consumer standpoint and a data collection business. The potential value of constant data collection through connected devices and backend algorithms and analytics to evaluate global health is enormous. This is borne out in the data- the dollars invested and number of deals VCs have made into digital health startups has been steadily increasing over the past decade.
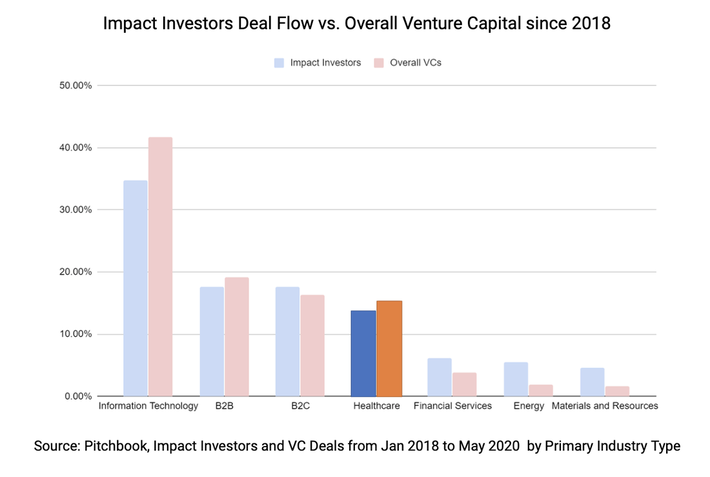
What we haven’t seen is investment from impact investors reflective of the importance of this domain to LMI communities. Analyzing the 478 impact investors and their associated 2.8k deals since 2018 shows that the share of VC healthcare deals were 13% higher than that of impact investors(11). Impact investments in healthcare trailed well behind those in energy, microfinance, and housing(12). This very well may stem from preconceived opinions on traditional life sciences- that they are high risk and capital intensive ventures. Impact investors are already often saddled with the misguided assumptions that they will provide below-market return; there is minimal appetite for layering on another potential high risk asset class. In reality, this new age of digital health services operates like the larger tech ecosystem. Leveraging AI and prediction algorithms, doctors are able to minimize the costly trial-and-error chapter of product development through simulation; furthermore, non-invasive diagnostics also eliminate the cost of expensive regulatory trials because the physical risk to patients is erased.
The impact of not being at the table cannot be understated. Medical professionals misdiagnose millions of US patients a year due to cognitive biases that plague all humans (e.g. anchoring, wishful thinking, confirmation, availability)(13). Similarly, AI algorithms are simply a reflection of the data used to develop them and are therefore subject to any underlying predilections. As already established, historical health data is likely biased due to utilization issues and leveraging that data set as ground truth will only serve to exacerbate existing prejudices and inequities at a global scale. Optum’s algorithm to predict health risk to allocate additional resources leveraged patient’s health care spending as a proxy for medical need, failing to account for different consumption behaviors across race; specifically, the result was that African-American patients only received additional help 17.7% of the time, as opposed to 46.5%(14) if this underlying bias was remedied.
Diversity on teams is also a common product development refrain as a factor that limits the efficacy of end solutions. Yet, products around the world clearly violate this principle. Examples such as soap dispensers that fail to work on darker shades of skin(15) and common asthma treatment recommendations not being optimized for African-Americans(16) make it clear that diversity is not always included in the ideation phase or clinical trials, let alone product design. And this is even clearer in healthcare providers where minorities make up 32% of patients, but only hold 11% of executive leadership positions at hospitals(17). In continuing to build these tech solutions, public good is only derived if diverse teams and integrated data sets are leveraged, despite the associated financial hurdles or operational obstacles. Not only will addressing these biases early lead to better end patient results, but these companies will also fare better in the market in the long-run, increasing ROI potential.
Takeaways
AI diagnostics presents a unique opportunity to not only improve affordability and effectiveness for patients, but also solve for many of the barriers to healthcare that plague those in LMI communities. Preventative care that focuses on non-invasive, data-based procedures will result in widespread impact, but in order to reach these lofty goals, there exists a clear need to continue highlighting the importance of inclusivity within healthcare AI. Whether in an advisory role promoting management team diversity or anchoring the technology in equitable data and processes, investors need to be able to flag these concerns to these firms. For those concerned about investing directly into life sciences startups without the requisite background, investing as an LP through other funds remains a viable alternative. Investing in funds that back these types of diagnostic technologies serves to mitigate risk, while requiring these impact metrics be included as core KPIs within these businesses.
About the author: Eddie Chan is a MBA Candidate at the Kellogg School of Management, holds a BA and BSE from the University of Pennsylvania, and is currently a Fellow at DigitalDx Ventures, an early-stage venture capital firm focused on digital diagnostics, and a Fellow at Impact America Fund, an early-stage venture capital firm focused on economic agency in low- to moderate-income communities. Before graduate school, he spent five years within Google and YouTube developing products and programs to democratize digital marketing and empower the next generation of content creators around the world.
Diversity on teams is also a common product development refrain as a factor that limits the efficacy of end solutions. Yet, products around the world clearly violate this principle. Examples such as soap dispensers that fail to work on darker shades of skin(15) and common asthma treatment recommendations not being optimized for African-Americans(16) make it clear that diversity is not always included in the ideation phase or clinical trials, let alone product design. And this is even clearer in healthcare providers where minorities make up 32% of patients, but only hold 11% of executive leadership positions at hospitals(17). In continuing to build these tech solutions, public good is only derived if diverse teams and integrated data sets are leveraged, despite the associated financial hurdles or operational obstacles. Not only will addressing these biases early lead to better end patient results, but these companies will also fare better in the market in the long-run, increasing ROI potential.
Takeaways
- Support for low- and moderate- income communities needs to broaden to all domains that impact the poverty cycle (education, employment, nutrition, healthcare)
- AI diagnostics represent a highly scalable technique for affordable and pervasive preventative healthcare - especially for communities that currently underutilize traditional infrastructure
- Impact venture investors need to increase their investments in this space, otherwise the peril is that the same systematic inequalities will be replicated at a global scale
AI diagnostics presents a unique opportunity to not only improve affordability and effectiveness for patients, but also solve for many of the barriers to healthcare that plague those in LMI communities. Preventative care that focuses on non-invasive, data-based procedures will result in widespread impact, but in order to reach these lofty goals, there exists a clear need to continue highlighting the importance of inclusivity within healthcare AI. Whether in an advisory role promoting management team diversity or anchoring the technology in equitable data and processes, investors need to be able to flag these concerns to these firms. For those concerned about investing directly into life sciences startups without the requisite background, investing as an LP through other funds remains a viable alternative. Investing in funds that back these types of diagnostic technologies serves to mitigate risk, while requiring these impact metrics be included as core KPIs within these businesses.
About the author: Eddie Chan is a MBA Candidate at the Kellogg School of Management, holds a BA and BSE from the University of Pennsylvania, and is currently a Fellow at DigitalDx Ventures, an early-stage venture capital firm focused on digital diagnostics, and a Fellow at Impact America Fund, an early-stage venture capital firm focused on economic agency in low- to moderate-income communities. Before graduate school, he spent five years within Google and YouTube developing products and programs to democratize digital marketing and empower the next generation of content creators around the world.
(1) What is the current poverty rate in the United States?
(2) 2017 Federal Poverty Level Guidelines
(3) Economic Security Programs Cut Poverty Nearly in Half Over Last 50 Years
(4) Dynamics of Economic Well-Being: Poverty 2009-2011
(5) Transitioning In and Out of Poverty
(6) The risk of falling into poverty after developing heart disease: a survival analysis
(7) Impact Of Diagnostics On Healthcare Outcomes
(8) In Health, Income Has Greater Impact than Race
(9) How Are Income and Wealth Linked to Health and Longevity?
(10) Use of AI for Detection, Diagnosis and Treatment of Mental Health Disorders
(11) Are you developing an impact measurement strategy?
(12) Impact investing: a new way to fund cures for cancer - STAT
(13) How 4 types of cognitive bias contribute to physician diagnostic errors — and how to overcome them
(14) Dissecting racial bias in an algorithm used to manage the health of populations
(15) Whites Only?
(16) African American children may need different asthma treatments
(17) Fostering diversity for the next generation of healthcare leaders
(2) 2017 Federal Poverty Level Guidelines
(3) Economic Security Programs Cut Poverty Nearly in Half Over Last 50 Years
(4) Dynamics of Economic Well-Being: Poverty 2009-2011
(5) Transitioning In and Out of Poverty
(6) The risk of falling into poverty after developing heart disease: a survival analysis
(7) Impact Of Diagnostics On Healthcare Outcomes
(8) In Health, Income Has Greater Impact than Race
(9) How Are Income and Wealth Linked to Health and Longevity?
(10) Use of AI for Detection, Diagnosis and Treatment of Mental Health Disorders
(11) Are you developing an impact measurement strategy?
(12) Impact investing: a new way to fund cures for cancer - STAT
(13) How 4 types of cognitive bias contribute to physician diagnostic errors — and how to overcome them
(14) Dissecting racial bias in an algorithm used to manage the health of populations
(15) Whites Only?
(16) African American children may need different asthma treatments
(17) Fostering diversity for the next generation of healthcare leaders